For centuries, it was the conventional narrative that leprosy, also known as Hansen’s disease, was introduced into the Americas by European colonists or enslaved Africans. But a groundbreaking new study published in Science is now overturning that assumption. According to an international team of researchers, a lesser-known bacterial species, Mycobacterium lepromatosis, existed across the Americas at least 1,000 years before European contact, rewriting our understanding of the disease’s global history.

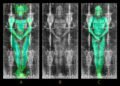
Led by scientists from the Paris Institut Pasteur, CNRS, and the University of Colorado, in collaboration with Indigenous communities, this study analyzed nearly 800 ancient and modern DNA samples from individuals across North and South America. The scientists discovered M. lepromatosis in human remains from as far apart as northern Canada and southeastern Argentina, areas more than 10,000 kilometers apart. All three examples were around a thousand years old, and the genomes were found to be surprisingly similar, which suggests a rapid, continent-wide spread of the pathogen in just a few hundred years.
“This discovery transforms our understanding of the history of leprosy in America,” said Dr. Maria Lopopolo of the Institut Pasteur, the study’s first author. “It shows that a form of the disease was already endemic among Indigenous populations well before the Europeans arrived.”
The bacterium M. lepromatosis was first identified in 2008 by Dr. Xiang-Yang Han and his colleagues at the University of Texas MD Anderson Cancer Center, following their discovery of it in two Mexican patients. Since then, cases have been reported all over the Americas, and in isolated incidents in Asia and the UK. Perhaps one of the most puzzling findings was in 2016, when veterinarians discovered M. lepromatosis in red squirrels in the British Isles. Genetic studies now indicate that this strain is likely to have originated in the Americas and could have been transported to Europe during the 19th century by human or trade activity.

The new study also examined 408 modern cases from Mexico, Brazil, and the U.S. They found that most of today’s strains are nearly identical to those in the ancient samples, which lends evidence to the long-standing and stable presence of the bacterium in the Americas. One exceptionally uncommon strain, genetically unique and ancient, was even identified in a living patient in North America, suggesting that potentially more than one lineage of M. lepromatosis may still be active today.
As Dr. Nicolás Rascovan, head of the Laboratory of Microbial Paleogenomics at the Institut Pasteur and study lead author, suggests, the discovery “clearly illustrates how ancient and modern DNA can rewrite the history of a human pathogen and help us better understand the epidemiology of contemporary infectious diseases.” He noted the necessity of continued surveillance, particularly in view of antimicrobial resistance as a growing global health challenge.
Interestingly, given the wide historical presence of the bacterium, physical evidence in ancient skeletons has been scarce. Unlike M. leprae, which causes distinctive bone lesions, M. lepromatosis damages blood vessels and internal organs such as the liver and spleen.

The researchers were careful to conduct their work in an ethical way, especially when they worked with ancestral remains. Indigenous peoples were involved in decision-making, and DNA data were shared following protocols designed to respect their cultural expectations. Materials were also returned to communities in some cases when requested.
The origins of M. lepromatosis are uncertain. Genetic information shows that it diverged from M. leprae between 700,000 and 1 million years ago. Whether or not the bacterium arrived in the Americas with early human migrations across the Bering Land Bridge, or evolved in native animal hosts and then spread to humans, is not yet determined, but what is known now is that the American roots of the disease run far deeper than previously suspected.